AI-powered notetaker for mental health professionals
An AI-assisted notetaking system accessible in both video and in-person sessions that records audio, generates transcripts, and converts them into structured clinical notes using industry-standard templates.
B2B2C
AI
Mental Health Tech
TEAM
Product Designer

Christine Chow
Product Managers
LA
MC
Developers & QA
NM
RM
Clinical Advisors
NS
SB
timeline
Sep – Oct 2025 (2 months)
Skills & tools
UX Research
UI/UX Design
Prototyping
Figma (Design / Make)
ChatGPT
at a glance
Context
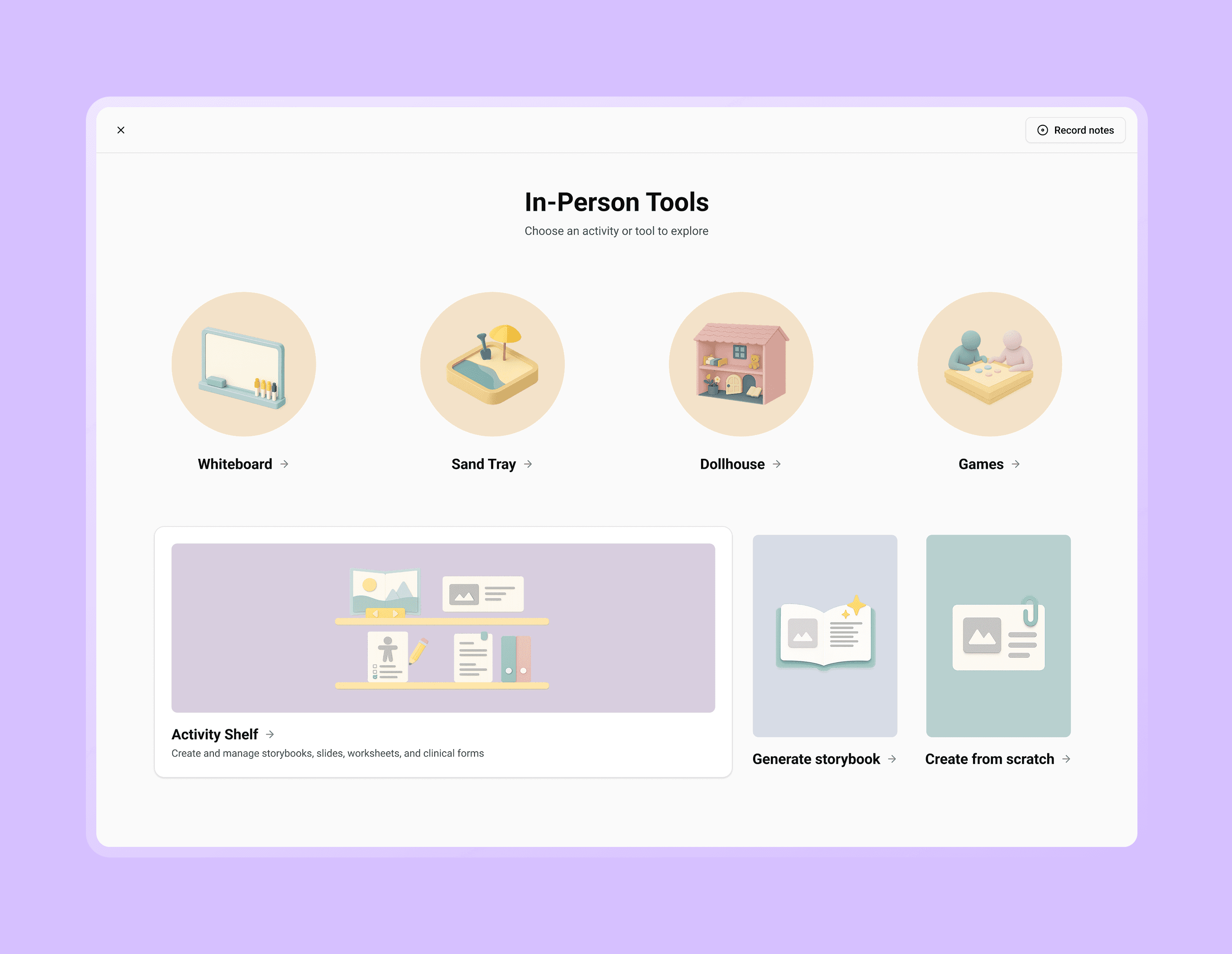
PlaySpace is an all-in-one platform for mental health professionals, combining practice management with interactive tools to deliver personalized and therapeutic activities for both in-person and virtual care.
Challenge
While preparing for broader market expansion, the team realized we needed more robust clinical documentation tools for practitioners who were drowning in administrative work in order to stay competitive.
According to a survey we sent out to 70 customers, 21.1% of respondents believed an AI-assisted notetaker would be helpful for their practice.
Impact
Created a custom design system
Using an open-source component library as a foundation, I delivered a usable lightweight design system in less than 2 months to ensure brand awareness and consistency across the platform.
Established Figma as our single source of truth
I onboarded the product and engineering teams to Figma; organized all design iterations. feedback, and comprehensive design documentation for a smooth handoff to developers; and recorded development inconsistencies to ensure design accuracy.
Lead regular interviews with clinical practitioners
As the sole product designer, I led weekly meetings with clinical advisors and regularly consulted the customer service team to validate designs with real workflows & pain points.
features
1 / 4
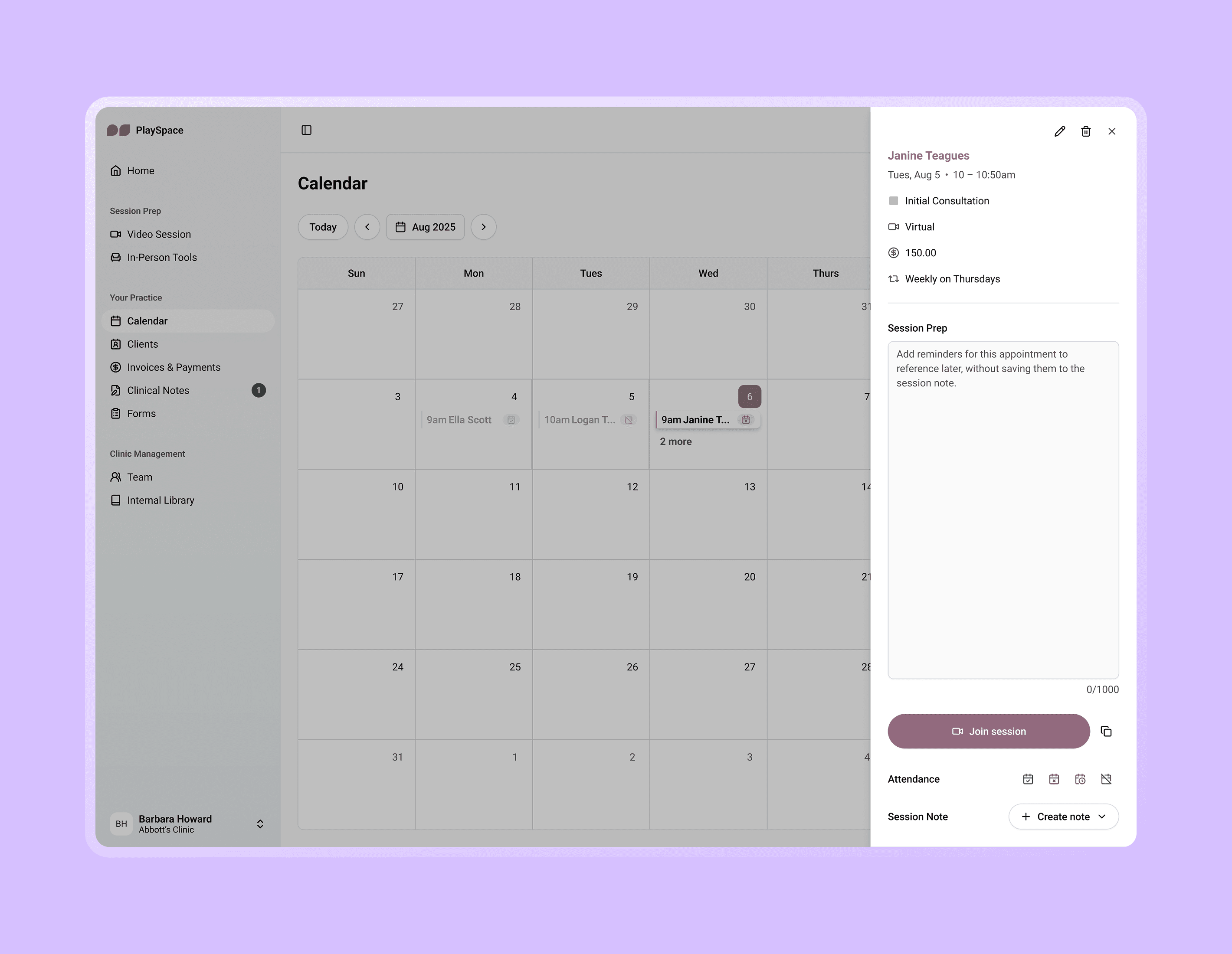
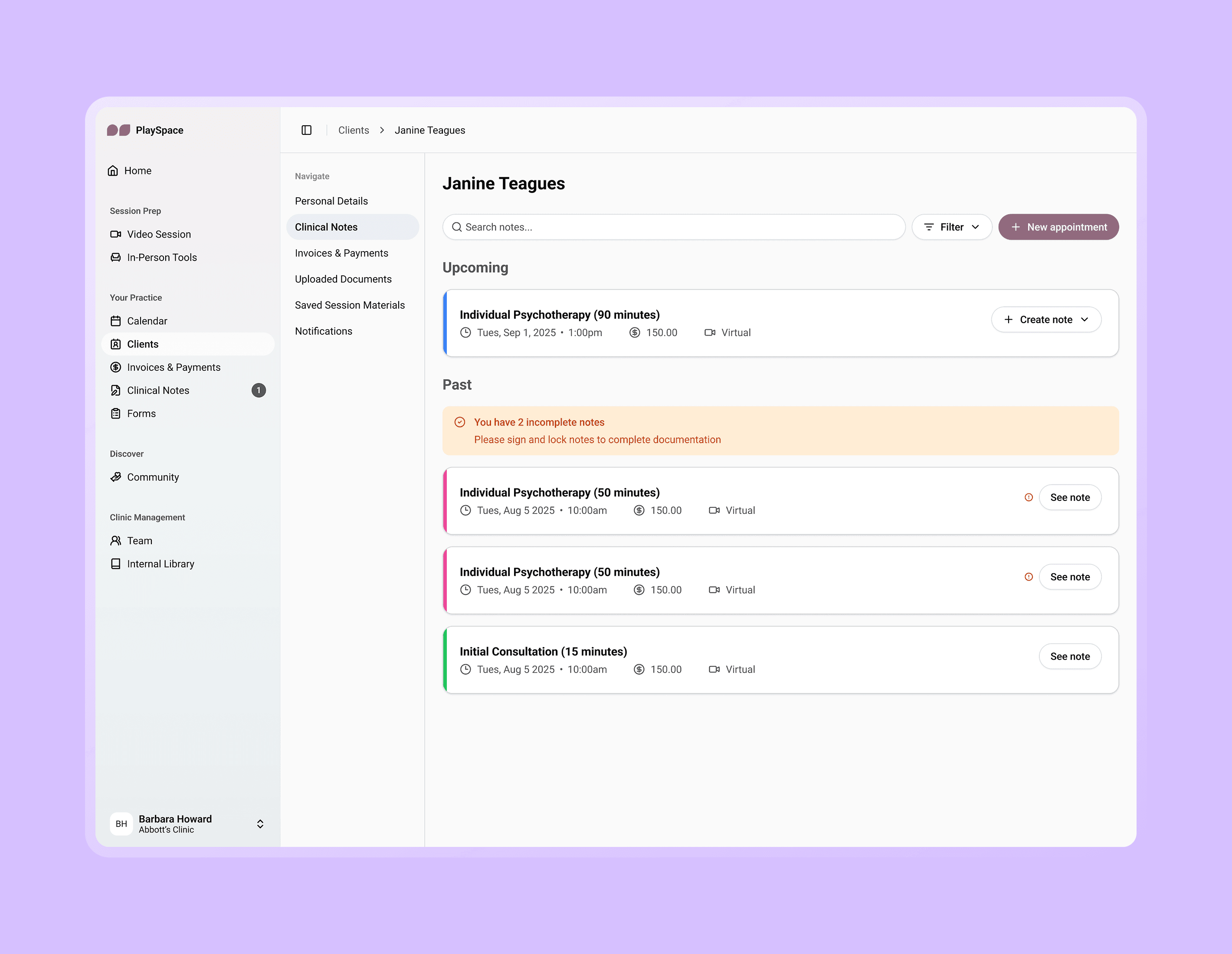
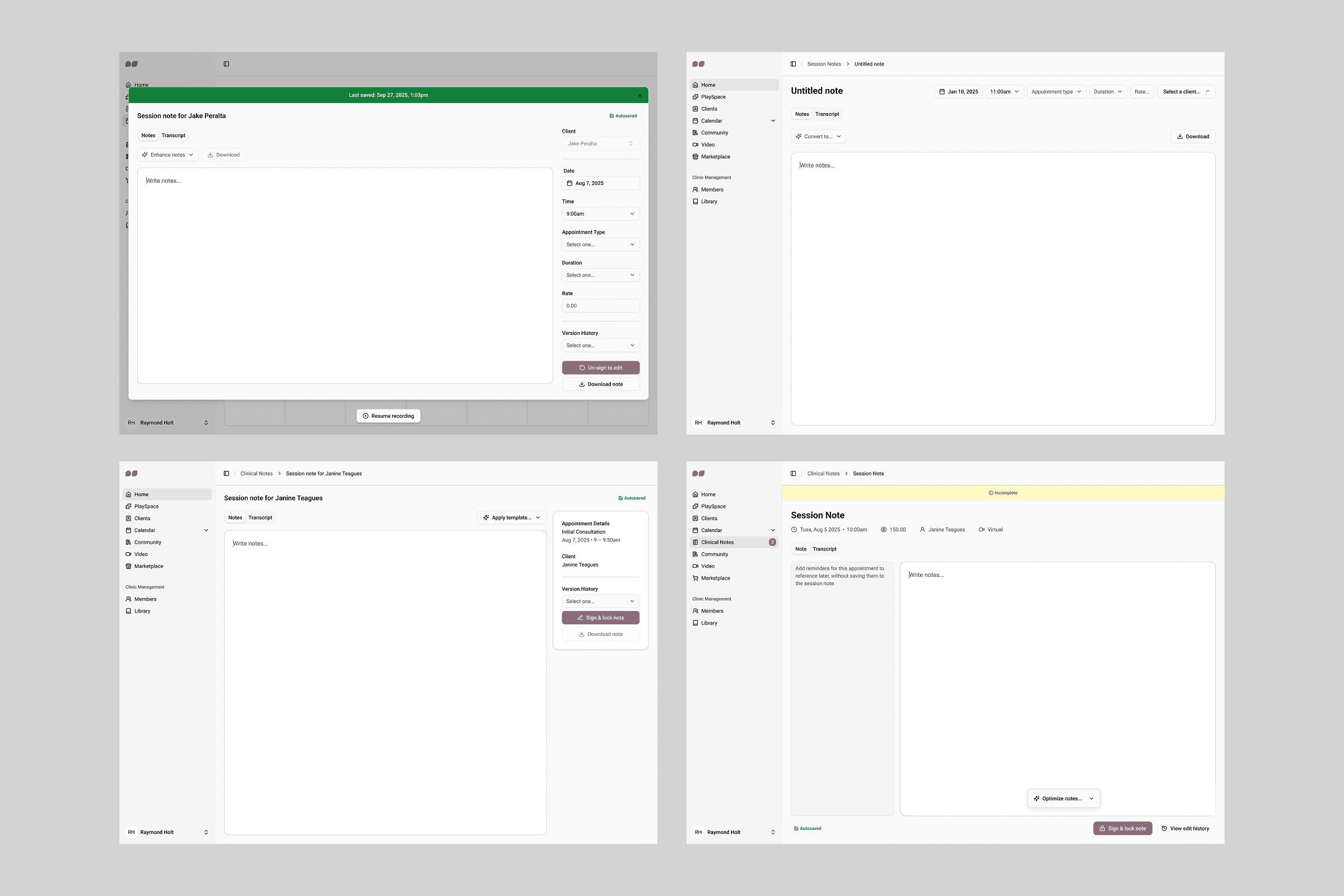
Multiple entry points for different workflows
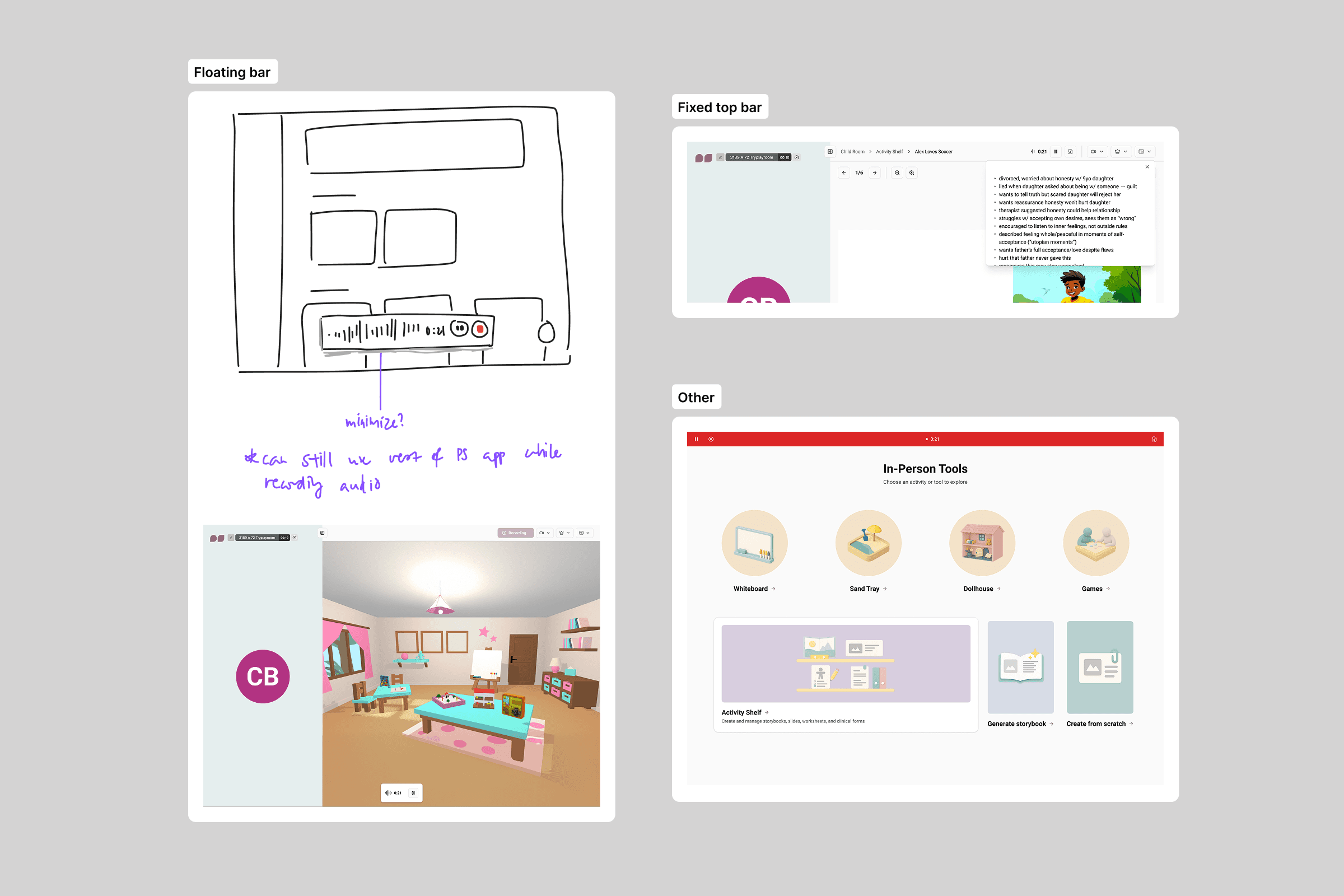
We had identified two potential user types: practitioners using PlaySpace as their primary EHR, and practitioners using PlaySpace alongside their own primary EHR. Because of this, I considered multiple entry points so our note-taking tool could adapt to fit different practices.
2 / 4
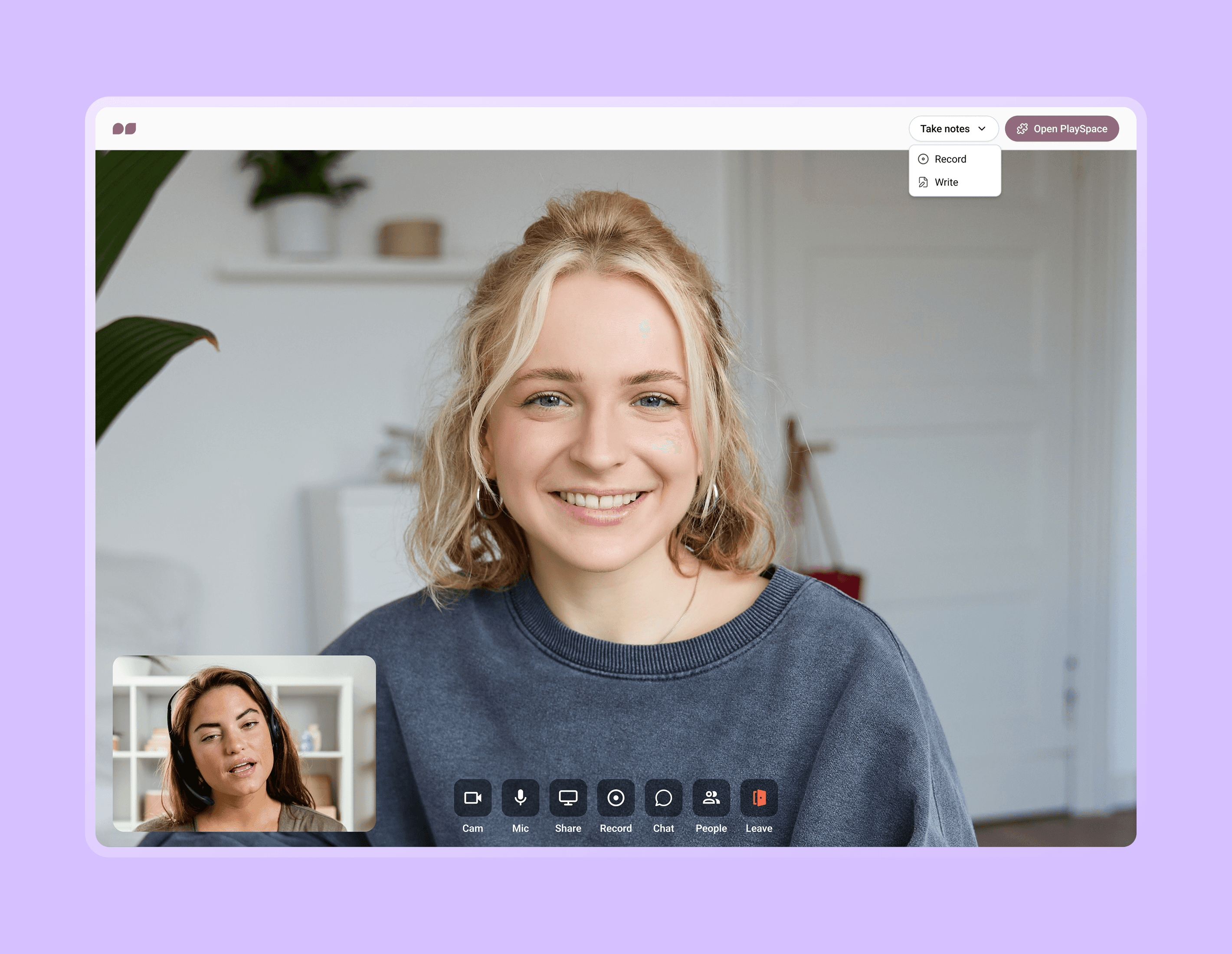
Notetaking in virtual sessions
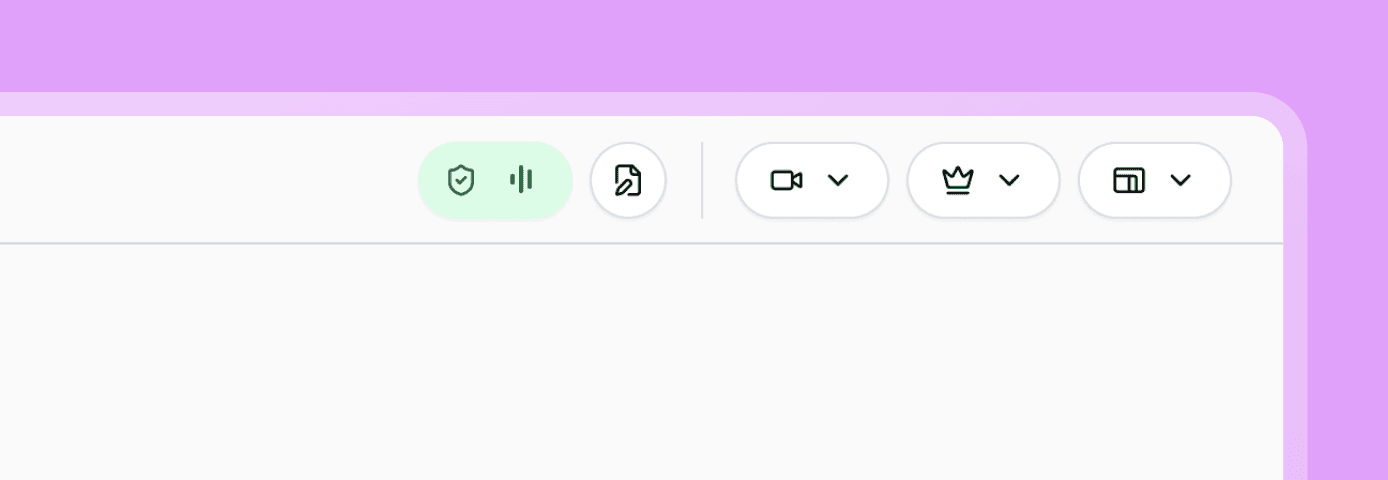
In a virtual session, practitioners can choose between taking notes without recording, or recording with quick notes — both options exist to give practitioners a sense of true ownership over their notes.
The quick notes interface is particularly designed to fit on the side, ensuring uninterrupted access to therapeutic tools and the client’s face.
During a recording, practitioners see a live indicator in the top bar while clients see a more subtle status.
3 / 4
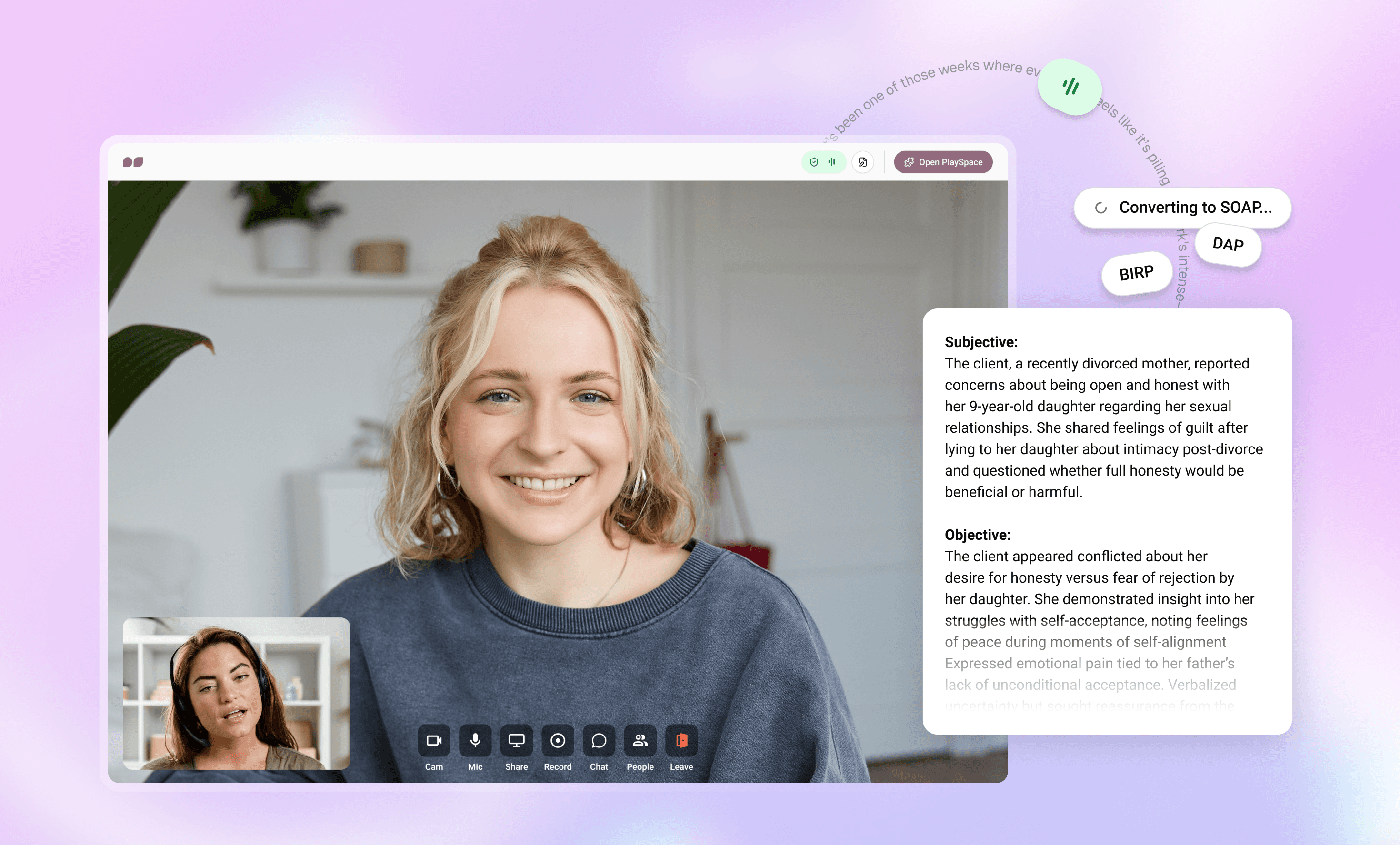
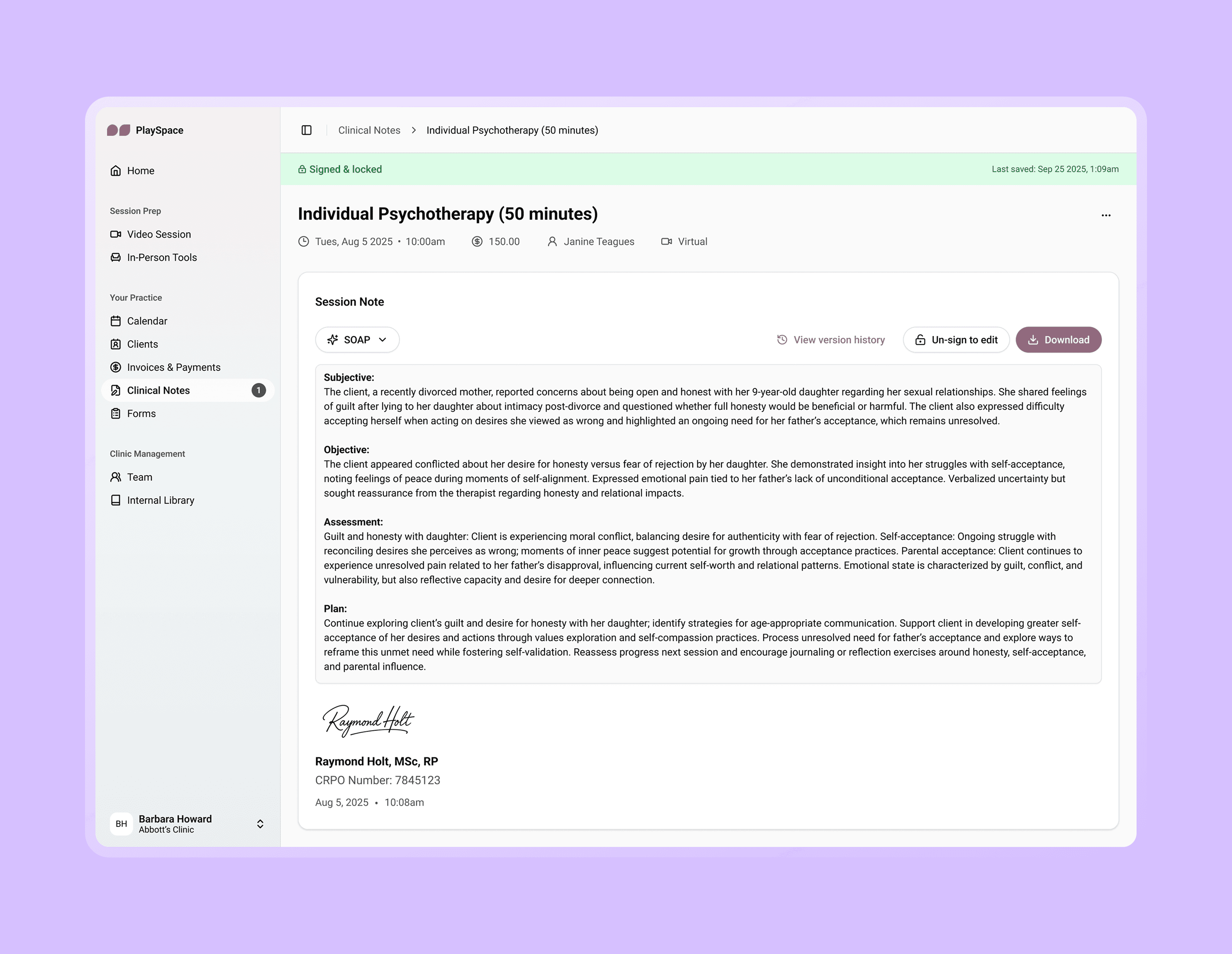
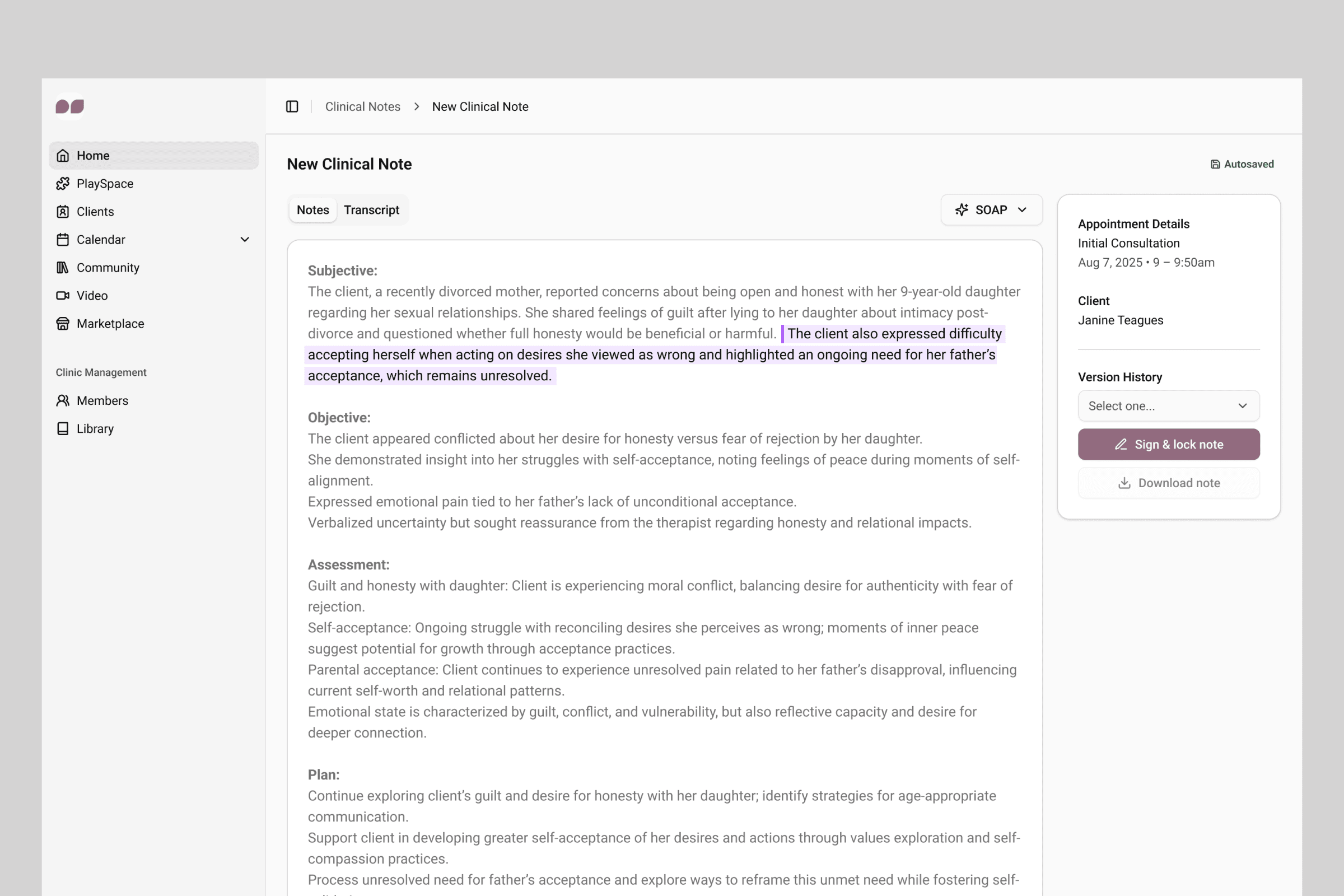
From session to official documentation
After the session, default templates are automatically applied to help practitioners complete the official session note, with relevant supporting documentation available on the side for reference.
Industry standard templates (SOAP, DAP, BIRP) are offered out of the box, with the option to create custom templates tailored to individual preferences.
4 / 4
Signing & locking the official note
Incomplete session notes must be signed and locked with the practitioners’ signature, full name, credentials, and date and time.
Research & Discovery
While navigating an ambiguous opportunity space with emerging technologies, I led the discovery work to help define the right scope and priorities for the challenge. There were the basic objectives that were provided:
Support both in-person and virtual session recording without disrupting client care
Convert transcripts to clinical templates (SOAP, DAP, BIRP formats)
Ensure HIPAA compliance and legal documentation requirements
Over the course of several weeks, I conducted extensive research with support from the product team and facilitated regular user interviews with a practicing clinical advisor to understand:
Current documentation workflows and pain points
Legal and compliance requirements (HIPAA, consent, note retention)
Clinical template preferences and customization needs
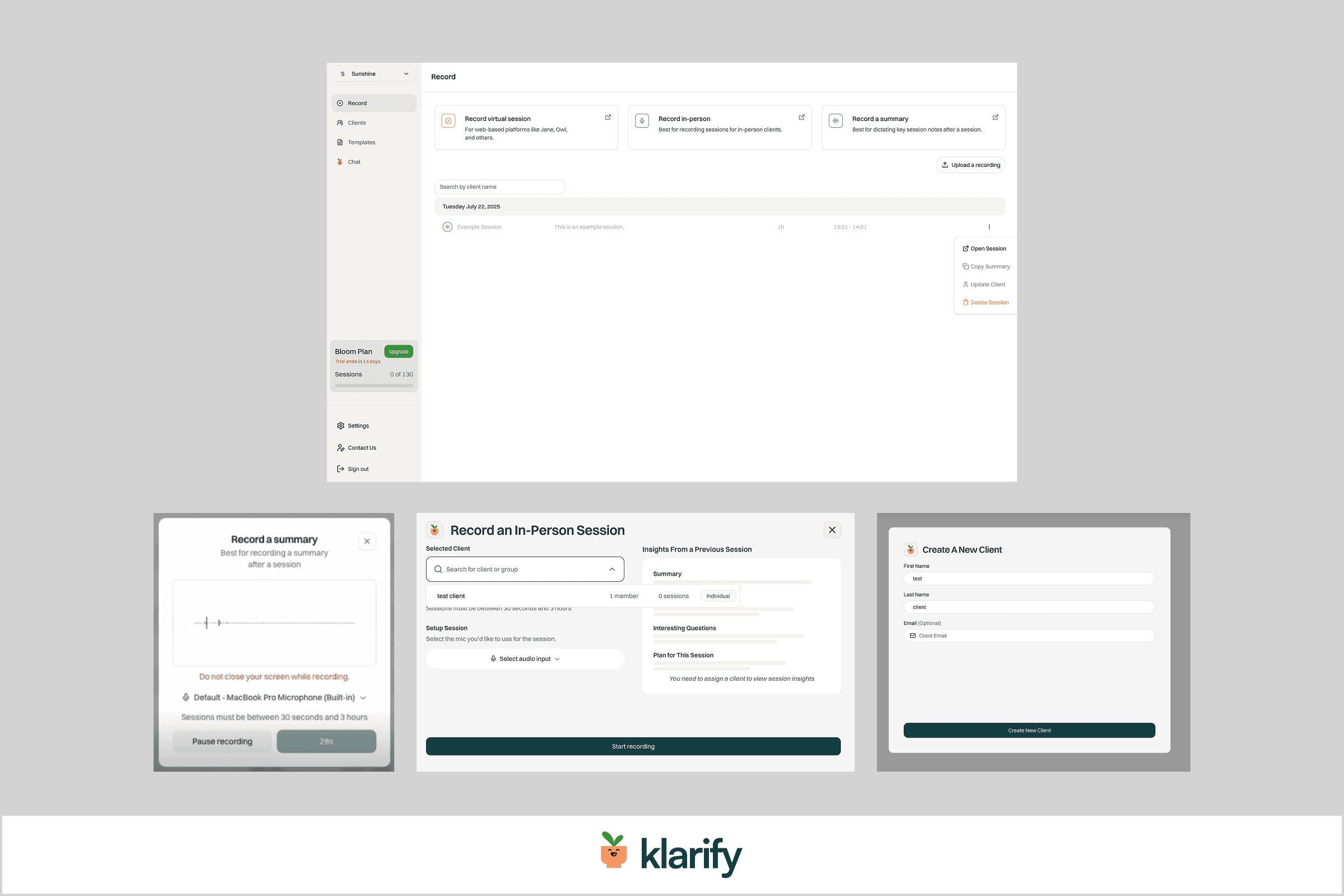
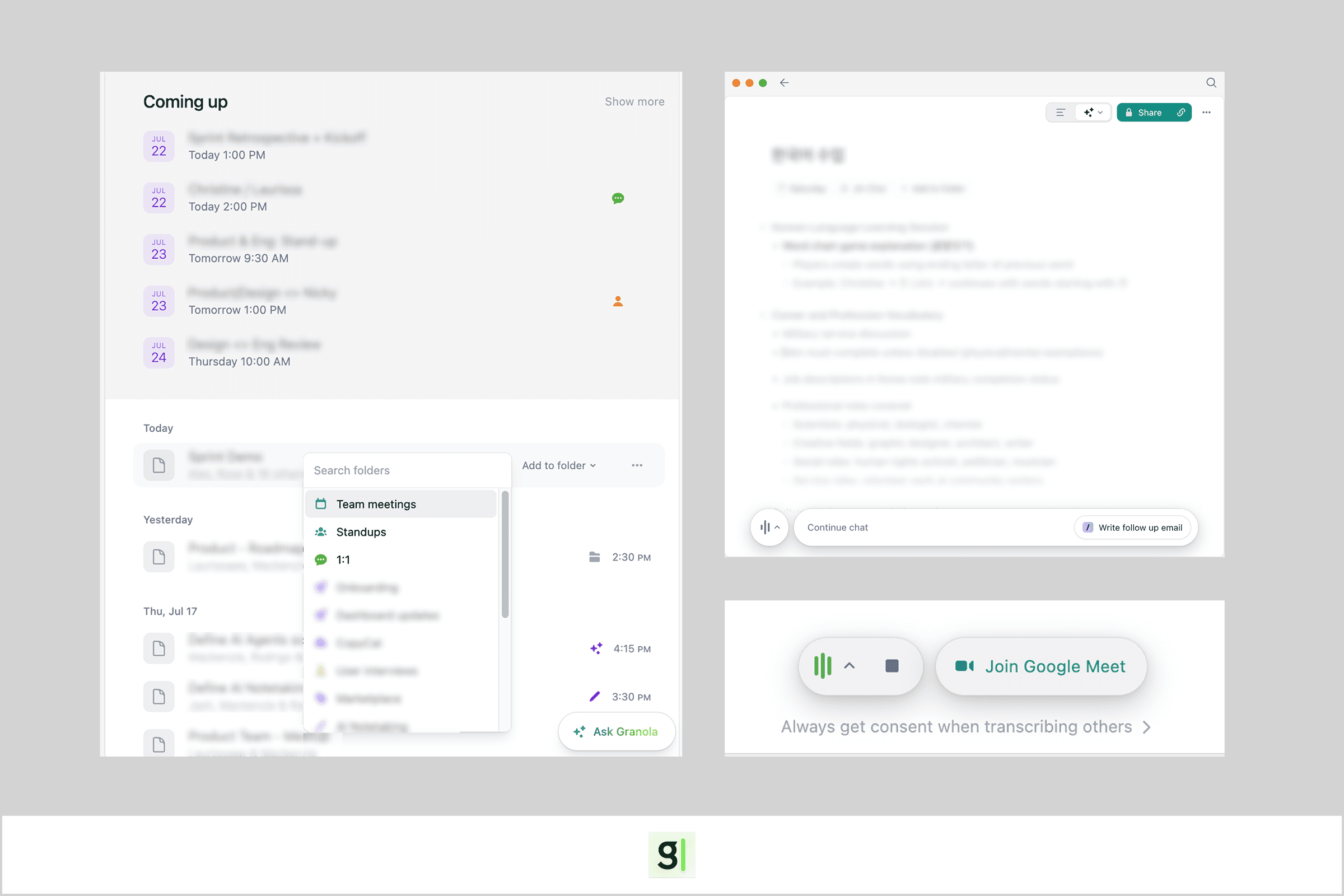
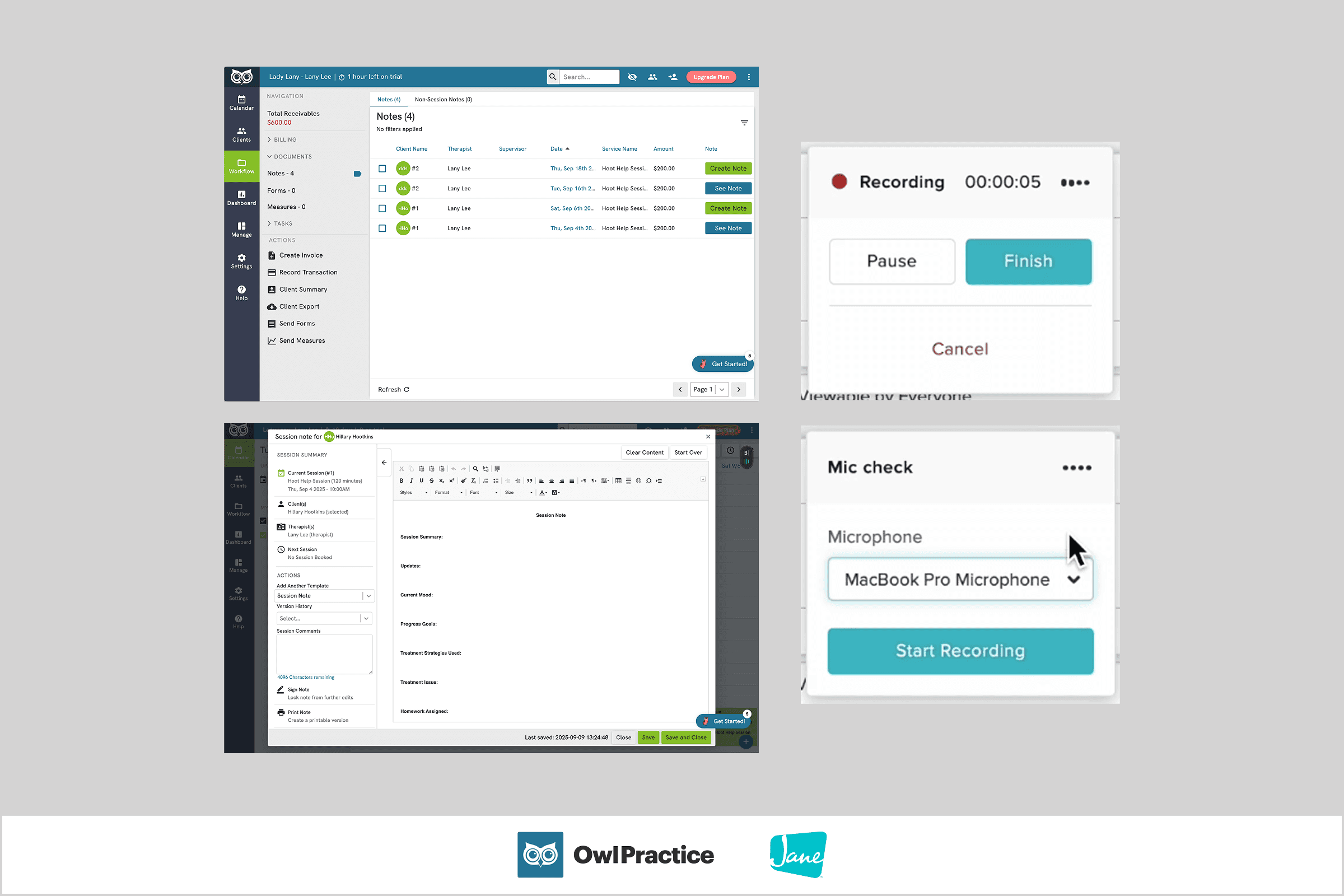
I also took inspiration from competitors:
Key Insights
1
Two distinct user types emerged
Practitioners using PlaySpace as their primary EHR might have different workflows from those using PlaySpace alongside their own EHR. Thus, each group might require different entry points for documentation flexibility.
2
Practitioners value personal ownership over their notes
Every practitioner has their own method: sparse notes vs detailed client quotes vs industry-standard templates, session prep vs no prep at all. This variety revealed 3 main design needs:
We must provide industry-standard templates out of the box, as well as support customized templates to cover all bases.
We had to clearly distinguish between the types of notes (Session Prep, Quick Notes, Official Session Note) to prevent confusion.
Many practitioners don't fully trust AI to handle sensitive client data, so we also needed to offer no-AI alternatives to help serve that group’s needs.
3
Legal compliance is critical
This meant properly handling consent, ensuring official session notes are properly signed and locked, and addressing concerns around client data duplication (especially for practitioners juggling multiple tools/systems).
design iterations